An ailing hip can make doing the things you love uncomfortable or even impossible. If you’re struggling with hip pain or stiffness that prevents you from performing everyday activities, you may find that hip replacement surgery could have a profound impact on your life. Hip replacement surgery can relieve your painful symptoms and increase your mobility and ability to function. However, conservative treatments are sufficient for some.
Below, you’ll find helpful information on hip replacement surgery and the signs that it’s a suitable treatment option for you.
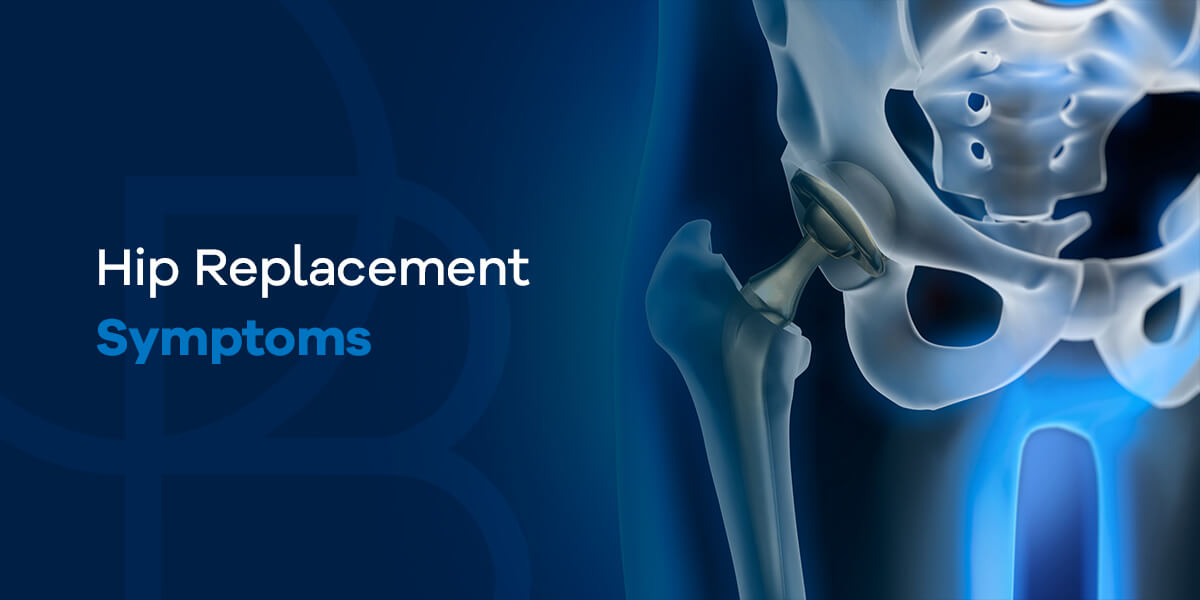
What Is a Hip Replacement?
Hip replacement is a surgery involving replacing damaged hip tissue with artificial implants or prosthetics. The main tissues involved with hip replacement are the ball and socket — the two bones that form the hip joint. The ball, called the femoral head, forms the top of the femur bone and the lower part of the hip joint. The socket, called the acetabulum, forms part of the pelvic bone and the top part of the hip joint.
Other tissues within the hip joint include:
- Hip ligaments: tough, fibrous tissues that bind bones together.
- Hip tendons: similar tissues to ligaments that bind muscles and bones together.
- Synovial fluid and membrane: membrane encapsulates the hip joint while the fluid lubricates it.
- Articular cartilage: covers the surface of the bones where they meet at the joint to reduce friction and allow for smooth motion.
- Hip muscles: support the hip joint and enable movement.
The implant consists of a ceramic ball and a titanium socket. The ceramic ball is attached to a metal stem that gets inserted into the femur bone to stabilize the artificial joint. The titanium cup is attached to the pelvic bone, letting the artificial hip joint move freely. In some cases, patients only need a partial hip replacement. In these cases, the surgeon only replaces the hip joint ball and leaves the socket as is.
There are three options for hip replacement surgery:
- Anterior hip replacement: The orthopedic surgeon accesses the hip joint from the front of the patient’s body.
- Lateral hip replacement: The surgeon accesses the joint from the patient’s side.
- Posterior hip replacement: As the patient lies face down or on their side, the surgeon accesses the hip joint from the back.
During hip replacement surgery, you receive either general anesthesia to relieve pain or an epidural which numbs all sensation below the waist. Once the anesthesia takes hold, the surgeon accesses the hip joint through the side, front or back. To begin, they remove the femoral head and create an opening in the femur’s center. Then, they will insert the stem into the opening before attaching the replacement ball to the stem.
After implanting the ball and stem prosthesis, the surgeon will remove the damaged cartilage from the socket part of the joint and attach the titanium cup. While you’re under anesthesia, the surgeon will bend and move your leg to ensure the artificial hip joint functions properly. They will use dissolvable sutures to close the soft tissues and surgical glue for the skin around the joint. Once you’re stitched up, they’ll wheel you to a recovery room where you’ll rest until discharge.
8 Signs to Know if You Need a Hip Replacement
How do you know if hip replacement is the right option for you? Let’s take a look at eight signs that will help you decide if you need hip replacement surgery.
1. You Have Chronic and Significant Pain
Damage to your hip joint can cause chronic and significant pain anywhere between your hip and knee. If you experience any of the following, you should talk to an orthopedic specialist immediately:
- You regularly take painkillers to deal with the pain.
- Your pain keeps you awake at night despite the use of pain medications.
- Your pain makes it difficult to walk or bend over.
- Your pain isn’t relieved by rest during the day or night.
- Conservative treatments have not helped your pain.
- You compensate for your pain with a limp.
- You rely on a walking aid to relieve your hip pain.
A primary reason patients avoid hip replacement surgery is that the recovery period causes limited activity. So if your pain is already severely limiting your activity, it makes more sense to have surgery to restore function to your hip joint. Severe pain is one of the main reasons patients seek a hip replacement, but it isn’t the only symptom that could indicate your need for hip replacement surgery.
2. Your Hip Disability Makes Completing Routine Tasks Difficult
The most important factor you should keep in mind when you’re deciding if you should have hip replacement surgery is how much your injured hip is affecting your life. Even if you can manage the pain, significant disability of the hip joint can make even the most routine tasks difficult or impossible, such as:
- Putting on your shoes or socks
- Walking normal distances
- Standing on one leg, even with assistance for balance
- Inability to move or bear weight on the affected leg
3. Hip Stiffness Limits Your Normal Range of Motion in the Joint
Stiffness is another indication that your hip may be severely injured and need hip replacement surgery. If you find that you’re experiencing joint stiffness that makes walking or bending your hip joint difficult or you can’t lift your leg, speak with an orthopedic specialist as soon as possible. While acute hip stiffness is normal if you’ve experienced an injury, chronic hip stiffness warrants prompt medical attention. Acute hip stiffness occurs suddenly and goes away in a short time. In contrast, chronic hip stiffness persists indefinitely.
4. Conservative Treatments Do Not Adequately Relieve Hip Pain
Many people with conditions affecting the hip joint, such as arthritis, do not need hip replacement surgery immediately. Your doctor will probably attempt conservative treatment options initially, including:
- Physical therapy: Strengthens and stabilizes muscles surrounding the hip joint and preserves or restores the hip’s range of motion, at least partially.
- Steroid injections: Reduces swelling and blocks pain signals.
- Anti-inflammatory medications: Reduces inflammation in the hip joint, which can relieve pain.
- Acupuncture: Promotes increased blood flow to the injured area to aid healing, relax muscles and reduce inflammation.
These treatments do not cure hip conditions. However, they can improve function and make hip pain more tolerable. Unfortunately, there may come a point when these conservative measures become less effective and fail to provide relief. When that happens, your doctor may suggest hip replacement surgery. Unless hip pain is unbearable, doctors recommend these conservative measures before opting for surgery.
5. Tests Reveal Advanced Arthritis or Significant Joint Damage
Your hip is a ball-and-socket joint. Cartilage and synovial fluid reduce the friction where the pelvic bone socket and the femoral head join. The cartilage wears away with hip osteoarthritis (OA), causing pain and joint damage. There’s no cushion between the bones rubbing together without cartilage, and they begin to wear down and damage the joint. Advanced cases of joint damage may make surgery necessary.
6. Joint Pain Is Wearing You Down Emotionally and Mentally
The physical ramifications of hip joint pain are obvious, affecting your ability to move and perform actions. However, chronic joint pain can also take a toll on a patient’s emotional and mental well-being. Even if you can tolerate your level of hip pain, after dealing with this symptom for months or even years, you may notice the signs of a mental health condition. In fact, chronic pain has been linked to depression and anxiety and shown to intensify the effects of preexisting mental illness.
7. You’ve Noticed Side Effects From Hip Pain Medications
Pain medications your doctor prescribes — such as NSAIDs — are relatively safe when you use them for a short amount of time. However, side effects can develop with prolonged use, including:
- Stomach irritation
- Ulcers
- Increased risk of stroke, blood clots and heart attack
- Weakened immune system
- Tolerance, which is when your body needs increasing amounts of the medicine to achieve the desired effect
- Addiction, which is when you experience notable withdrawal symptoms whenever you aren’t taking the medication
8. Less Complicated Surgical Procedures Are Unlikely to Help
A few other surgical procedures offer an alternative to hip replacement surgery. However, surgeons seldom perform them now that hip replacement has developed a high success rate among most patients. If your doctor seems doubtful that you’ll benefit from less complicated surgical procedures, you could be a leading candidate for hip replacement surgery. Often severe hip fractures fall under this category, especially for older adults.
Reasons Not to Have a Hip Replacement Surgery
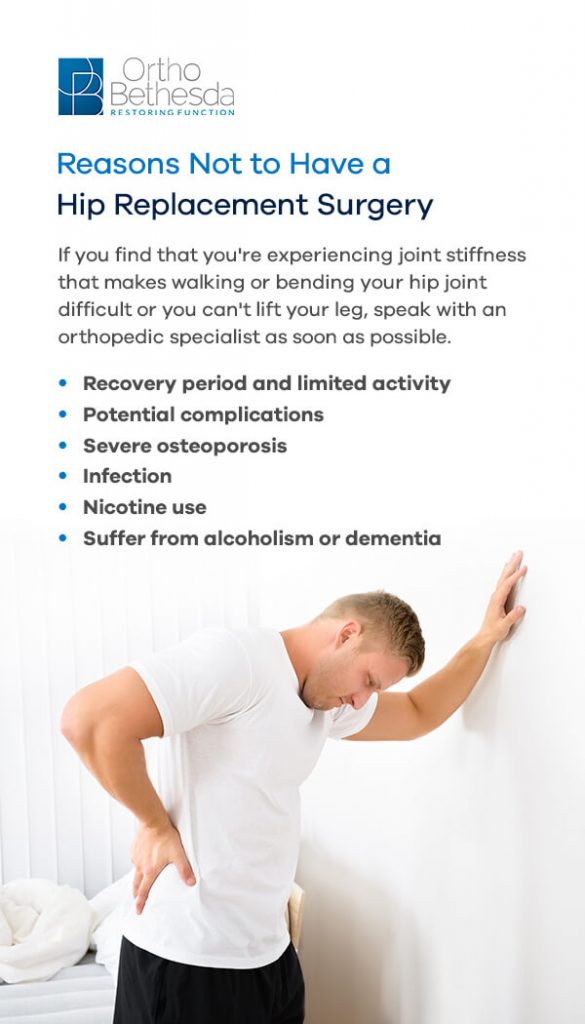
If you’re dealing with hip pain or other hip-related issues, hip replacement surgery is typically a last resort. As a last resort, there are many reasons to put off or avoid hip replacement surgery. If the hip issues you’re experiencing improve with less invasive treatment methods, hip replacement surgery is unnecessary. Various reasons exist for why doctors consider hip replacement surgery as a last resort, including:
- Recovery period and limited activity: Hip replacement surgery involves a lengthy recovery period with restricted activity levels. To avoid disruptions with work and your daily life, doctors often recommend less invasive treatments before broaching surgery as a possibility. If your hip issues cause significant disruptions to your everyday life, your best option may still be surgery.
- Potential complications: As with any surgery, there is potential for various complications, including bleeding, infection, blood clots or injury to nearby nerves. Potential complications unique to hip replacement surgery include possible fracture, dislocation, unrelieved joint pain and leg length discrepancy. Such complications are rare but not impossible.
- Severe osteoporosis: If you have severe osteoporosis, the risks of hip replacement surgery increase. Your bones may not support or adhere to the joint prosthesis in these situations. Your doctor may consider the risks of hip replacement outweigh the benefits if you have severe osteoporosis. They may also suggest steps to improve bone density before proceeding with hip replacement surgery.
- Infection: An infection is an absolute contraindication to hip replacement surgery. In such cases, your doctor will postpone the surgery until the infection clears.
- Nicotine use: Various studies show that nicotine use and smoking increase postoperative complication risks, particularly with implant surgeries. Thus, doctors advise patients to cease smoking tobacco or nicotine products a certain amount of time before surgery.
- Suffer from alcoholism or dementia: Individuals who suffer from alcoholism or dementia may be unable to adhere to the postoperative instructions involved with hip replacement surgery. Such instructions protect against further injury and postoperative complications. A doctor will weigh the benefits and increased risks in such situations.
Hip Replacement Surgery FAQ
Whether you’re in the thick of hip replacement recovery, anticipating a hip replacement surgery or weighing your options, it’s common to have several questions. Here are some answers to frequently asked questions about hip replacement surgery.
Is a Hip Replacement a Major Operation?
Hip replacement surgery is a major operation. Major operations include any surgery where a surgeon creates an incision to open up the body and cause trauma to soft tissues. Since hip replacement surgery involves an incision and causes trauma to the ligaments, muscles and tendons surrounding the hip joint, it is major surgery. That said, minimally invasive options exist for hip replacement surgery that involve smaller incisions and less trauma to surrounding joint tissues.
How Long Are You on Bed Rest After a Hip Replacement?
After a hip replacement, patients remain in the hospital for approximately two to four days. Most of this time will be spent resting in a hospital bed. For the first two to three hours after hip replacement, the patient will remain in the recovery room exclusively under bed rest as they awake from the anesthesia. Most patients remain in a hospital bed until the following day, when they can get out of bed with assistance from a nurse and caretakers.
How Long Does It Take to Recover From a Hip Replacement?
Recovery length from a hip replacement surgery depends on various factors and can take anywhere from six months to one year. Some factors that influence how long it takes to recover from hip replacement surgery include:
- Your age, nutrition and physical condition.
- The type of procedure — whether it was partial or total hip replacement surgery.
- How closely you adhere to pre- and post-procedural instructions.
- Whether any complications occur during or after surgery.
- The strength of your bones and their ability to adhere to the prosthesis.
- Whether you qualify for minimally invasive hip replacement surgery.
The classic hip replacement recovery timeline is as follows:
- Day of surgery: Hip replacement surgery is an all-day affair. While the actual surgery takes approximately 2-3 hours, you’ll need to show up several hours before so nurses and doctors can prepare you for surgery with an IV. After surgery, you’ll likely be admitted for inpatient care and sent to a recovery room for a couple more hours to recover from anesthesia. You’ll have a liquid diet for the rest of the day and receive various IV medications to relieve pain and prevent blood clots and infection.
- 1-2 days after surgery: You’ll likely stay in the hospital for the next couple of days. You’ll rest in a hospital bed for the first 24 hours, after which you can get out of bed with help and move around for short periods with crutches or a walker. While you’ll need lots of rest, mobility is also important to keep your muscles strong and blood flowing to prevent blood clots. Physical therapists will help you move with the least amount of pain. You’ll also return to a regular diet and take oral medication.
- 3-4 days after surgery: Some patients can walk short distances without help after three days, despite some manageable pain. If you experience no complications during this time, you should be free to leave by the third or fourth day. Before you leave, your doctor will provide discharge instructions and ensure you have someone who can drive you home. It’s also advisable to have someone stay with you for several days or weeks, if possible.
- 4-10 days after surgery: Once you return home, you’ll need to take special care to avoid infection. Follow all of the surgeon’s instructions about caring for the incision site. Consistently check for signs of infection and let your doctor know if you see any. They include discharge oozing from the incision, fever, redness or swelling. You’ll need to avoid immersing the incision in water and rely on showers instead of baths. You should be mobile with light stretching and short walks to maintain strength, improve circulation and prevent stiffness.
- 10-14 days after surgery: Unless surgical glue and dissolvable sutures were used, your doctor will remove the staples during this time.
- 3-6 weeks after surgery: Within this timeframe, you may be able to resume light activity without an assistive walking device, as long as your surgeon clears you. You should also be able to return to work during this period unless your occupation is physically demanding.
- Ten weeks to one year after surgery: Within 10-12 weeks, you should be able to resume normal activity. Once you no longer need prescription pain medication to move around, your doctor will clear you for driving. Still, you’ll likely need 6-12 months before experiencing a complete recovery. It’s possible to experience minor pain after making a full recovery.
How Painful Is a Hip Replacement?
It’s normal to experience pain, swelling and tenderness in the hip joint after hip replacement surgery. Your pain shouldn’t consistently exceed a six on a 1-10 pain scale after hip replacement surgery, even if it occasionally reaches those levels. As you improve strength, flexibility and circulation with physical therapy, your pain levels should gradually subside to a one or two on the pain scale.
If you think your pain is excessive, speak to your doctor as soon as you can. Most patients experience discomfort in the hip, groin and thigh regions for 2-4 weeks after hip replacement surgery.
Which Method of Hip Replacement Is the Best?
The different hip replacement surgery methods have pros and cons and unique applications:
- Anterior hip replacement surgery: This approach enters the hip joint through the front of the upper thigh. The main benefit of this approach is that it works between muscles. With this approach, surgeons can access the hip joint without separating muscle from bone, which helps patients recover faster. That said, the anterior approach has a higher risk of causing nerve damage.
- Posterior hip replacement surgery: The posterior approach provides surgeons with more precise views of the hip joint. Yet, this approach also involves cuts through several muscles to access the joint. Since the posterior approach causes increased trauma to the surrounding tissues, this approach involves lengthier recovery times. That said, it may be necessary for complicated hip replacement surgeries. The posterior approach causes trauma to the top of the outer thigh muscles, the gluteus maximus and external hip rotators.
- Lateral hip replacement surgery: Like the posterior approach, lateral hip replacement surgery provides clearer views of the hip joint but has to cut through muscles to get there. The lateral approach affects the gluteus medius and minimus muscles. A surgeon would opt for this approach instead of the posterior if the damage mainly exists at the side of the hip joint.
Ultimately, each method has its merits, and the most important factor is the skill and expertise of the surgeon performing the procedure.
Meet Our Doctors Who Treat the Hip
If you struggle with severe hip pain or disability, you may be a candidate for hip replacement surgery. To find out if that’s an appropriate treatment option for you, contact the team at OrthoBethesda. Our highly skilled orthopedic specialists serve the community in and around Bethesda, MD, with compassionate care and can help you decide on the best treatment option for your hip pain. Call us today at (301) 530-1010.

Related Content
- Why Are Hip Fractures So Dangerous?
- How to Sleep After Total Hip Replacement Surgery
- When You Can Bend Over 90 Degrees After Hip Replacement
- How Long Does Hip Replacement Surgery Take?
- Robotic vs. Traditional Hip Replacement Surgery
- Anterior vs. Posterior Hip Replacement
- How to Keep Your Hips and Knees Healthy at All Stages of Life
