Shoulder problems are a common issue for many people. Let the OrthoBethesda team of highly-trained doctors and staff help you regain your mobility and reduce your pain.
Meet Our Doctors Who Treat the Shoulder






Shoulder Conditions and Treatments
Your shoulders are important joints in your body. The pain and discomfort you experience in your shoulder can be very uncomfortable. Let the OrthoBethesda Team diagnose and treat your shoulder condition so you can gain back the use and mobility of your shoulder.
Conditions:
Shoulder Basics
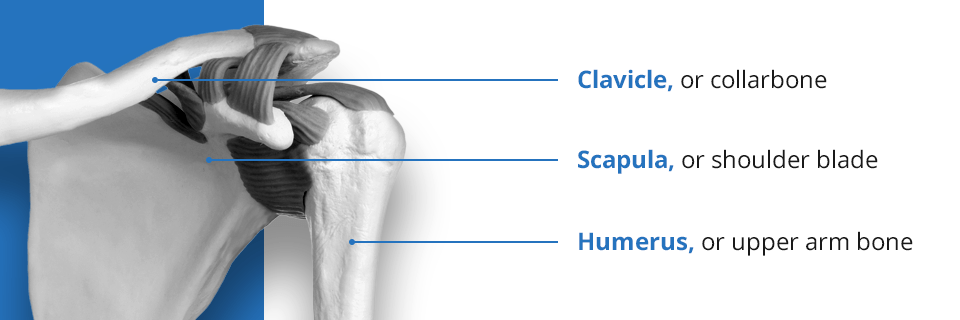
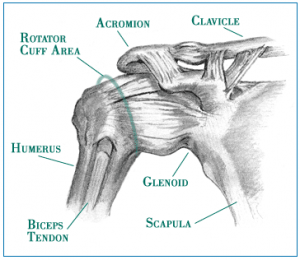
The shoulder is the most complex joint in the body. It is made up of three bones, the scapula (shoulder blade), the humerus (upper arm) and the clavicle (collar bone). There are four articulations, the AC (acromioclavicular) joint, SC (sternoclavicular) joint, GH (glenohumeral) joint and the scapulo-thoracic articulation. Finally, there are 13 muscles including the four of the rotator cuff. The rotator cuff muscles move our shoulders and also keep it centered in the socket. The rotator cuff muscles are the supraspinatus, whose primary function is to lift your hand over your head, the infraspinatus and teres minor both of which are external rotator’s of the shoulder and the largest muscle of the group is the subscapularis which is the primary internal rotator of the shoulder.
The shoulder is the least stable joint in the body. I liken the shoulder joint to a golf ball sitting on a golf tee. It is a very unstable system. When you tilt the golf ball just a little the ball will roll right off the tee. Why doesn’t our shoulder dislocate throughout the day with activities of daily living? Because there’s a complex system of passive and dynamic stabilizers to keep the ball (humeral head) centered on the socket (glenoid) no matter what position we put our arms in.
What do I mean by passive stabilizer? A passive stabilizer is a structure that keeps the shoulder from dislocating based upon the stabilizer’s shape, structure or location. One example is that the shape or curvature of the socket (glenoid) is the same as the much larger ball (humeral head). Furthermore, a thin film of joint fluid helps the ball stick to the socket. Next there is a rubber-like gasket or washer attached to the periphery of the glenoid called the labrum. The labrum is composed of cartilage and turns the socket into a suction cup. Injury to the labrum of the shoulder can cause painful clicking or worse – instability of the ball in the socket resulting in dislocation. Labrum injuries are associated with shoulder dislocations, overhead throwing or racket sports, and even just the aging process. Most patients over the age of 30 will have a labrum tear of some sort – SLAP tears, posterior labrum tears, degenerative tears, etc. Finally, the joint capsule is another passive stabilizer that acts like a shrink wrap around the shoulder joint. This shrink wrap creates negative pressure in the joint that sucks the ball (humeral head) into the socket (glenoid). Thickening in specific areas of the capsule are referred to as the glenohumeral ligaments. At extreme rotation the ligaments tighten and help to keep the shoulder centered in the joint.
What about the dynamic stabilizers? Dynamic stabilizers prevent the shoulder from dislocating by actively contributing. For example, the most important dynamic stabilizers are the 4 muscles of the rotator cuff. When working together in a normal fashion, they compress or hold the humeral head in the center of the glenoid no matter what position we put our hand in. Weakness due to tearing, inflammation or strains of the rotator cuff muscles will cause the humeral head to move around in the socket more than normal. This will not only cause pain, it can lead to a complete dislocation of the shoulder.
As you can see, the shoulder is a very complex joint. This is why almost everyone gets some sort of shoulder pain in their lifetime!
Guide to Shoulders
The shoulder is a ball and socket joint. The ball portion of the joint consists of the rounded head of the upper arm bone (humerus), and the socket portion is made up of a depression (glenoid) in the shoulder blade. The humeral head (ball) fits into the glenoid (socket) creating the joint that allows you to move your shoulder. The joint is surrounded and lined by cartilage, muscles, and tendons that provide support, stability, and ease of movement.
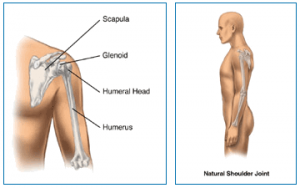
The shoulder allows for the rotation of the arm in all directions. The range of motion is dependent on the proper articulation of the humeral head upon the glenoid (shoulder socket).

Shoulder Replacement – Frequently Asked Questions
This following provides a brief introduction to shoulder replacement. It can help you make a list of questions to ask your doctor, but it is not meant to provide complete information. Check with your surgeon’s office about more comprehensive resources and patient education materials.
What is shoulder replacement?
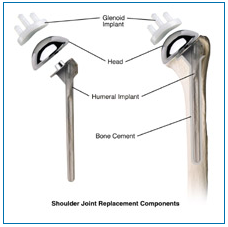
In shoulder replacement surgery, the painful surfaces of the damaged shoulder are resurfaced with artificial shoulder parts. The part that replaces the ball consists of a stem with a rounded metal head. The part that replaces the socket consists of a smooth plastic concave shell that matches the round head of the ball. When both sides of the joint are resurfaced, we call it a total shoulder replacement. However, your doctor may determine that only the humeral side of the joint (ball) should be resurfaced. We call this a partial shoulder replacement.
How do I prepare for shoulder replacement surgery?
If you and your surgeon decide that total shoulder replacement is right for you, a date will be scheduled for your surgery. Several things may be necessary to prepare for surgery. For example, your surgeon might ask you to have a physical examination by your primary care physician. This will ensure that other health problems you may have, such as diabetes or high blood pressure, will be treated before surgery. Your doctor, or a staff ember, will advise you about the things you can do to prepare for your hospital stay, and your rehabilitation after surgery.
What happens during shoulder replacement surgery?
One the day of surgery, an intravenous tube will be inserted into your arm to administer necessary medications and fluid during surgery. You will then be taken to the operating room and given anesthesia. After the anesthesia takes effect, your shoulder will be scrubbed and sterilized with a special solution that removes bacteria from your skin.
The procedure is performed through an incision over the shoulder that will expose the joint. Special, precision guides and instruments will be used to cut the humeral head (ball) and prepare the bone to accept the implant. The new metal ball and stem are then inserted. If the socket is to be resurfaced, its damaged surface is smoothed and the new plastic surface is inserted. The ball and socket are then joined. When the surgeon is satisfied with the fit and function, the incision will be closed and covered with dressings. A special drain may be inserted into the wound to drain the fluids that naturally develop at the surgical site. The surgery usually takes one to three hours, although this depends on the severity of the arthritis in your shoulder.
A sterile bandage will be placed over the wound, and you will be sent to the recovery room where you will be carefully monitored. As the anesthesia wears off you will slowly regain consciousness. A nurse will be with you, and may encourage you to cough or breathe deeply to help clear our lungs. Your arm will be in a sling or brace, and it may be wrapped in an ice pack to help control pain and swelling. You will also be given pain medication. When you are fully conscious, you will be taken back to your hospital room.
What can I expect after surgery?
When you are back in your hospital room, you will begin a gentle rehabilitation program to help relax the muscles around your new shoulder. On the day of surgery you may be encouraged to get out of bed and take a few steps. You will continue to receive pain medication as needed, and your bandage will be removed about two days after surgery.
Depending on your specific situation, you will probably remain in the hospital from one to three days. Your shoulder area may be warm and tender for several weeks. Before you are dismissed from the hospital, your physical therapist will show you how to perform the rehabilitation exercises that are important for your recover.
How soon can I return to normal activities after surgery?
Successful joint replacement surgery may relieve your pain and stiffness, and may allow you to resume some of your normal daily activities as instructed by your doctor. But even after you have fully recovered from your surgery, you may still have some restrictions. Normal daily activities for shoulder replacement patients do not include contact sports “jamming” activities such as hammering, repetitive heavy lifting, or activities that put excessive strain on your shoulder. Although your artificial joint can be replaced, a second implant is seldom as successful as the first.
How long will a shoulder replacement last?
Longevity of the prosthetic shoulder varies from patient to patient. It depends on many factors, such as a patient’s physical condition and activity level, as well as the accuracy of implant placement during surgery. It is useful to keep in mind that prosthetic joints are not as strong or durable as a natural, healthy joint, and there is no guarantee that a prosthetic joint will last the rest of a patient’s life.
Today, total shoulder replacement is becoming a common and predictable procedure. Many patients enjoy relief from pain and improved function, compared to their status before surgery. As a result, some patients may have unrealistic expectations about what the prosthetic shoulder can do and how much activity it can withstand. As with any mechanical joint, the ball and socket components move against each other. Natural fluid in the joint space, called synovial fluid, helps to lubricate the implants just as it lubricates the bones and cartilage in a natural joint. Still, the prosthetic components do wear as they roll and slide against each other during movement. As with car tires or brake pads, the rate of wear depends partly on how the shoulder joint is used. Activities that place a lot of stress on the joint implants, as may be the case with more active patients, may reduce the service life of the prosthesis. Implant loosening and wear on the plastic portions of the implant can lead to the necessity for revision surgery to replace the worn components, or all of the components. Your doctor will be in the best position to discuss these issues with you, taking into account your particular clinical circumstances, the type of implants used, and your post-surgical lifestyle.
Talk with your doctor about the following points, and how they might affect the longevity and success of your shoulder replacement:
- Avoiding repetitive heavy lifting
- Avoiding “jamming” activities such as hammering
- Staying healthy and active
- Avoiding “impact loading” sports such as boxing
- Consulting your surgeon before beginning any new sport or activity, to discuss what type and intensity of sport or activity is appropriate for you
- Thinking before you move
- Not lifting or pushing heavy objects
Rotator Cuff Disorders: The Facts
There is a great deal information circulating about the rotator cuff and its disorders. Some of this is due to misinformation in the lay press and unfortunately some of it has been disseminated by medical professionals either through a misunderstanding of current information or a desire to simplify the situation. This information sheet is meant to provide you with facts and where there are no facts, the best understanding that is currently available about these problems. I have relied on orthopaedic texts and information provided at the many courses that I have attended sponsored by the American Academy of Orthopaedic Surgeons.
The rotator cuff is a group of 4 tendons (tendons are the connection of muscles to bone) that connect to the head of the humerus (the ball of the ball and socket joint of the shoulder). It is made up of the subscapularis, the supraspinatus, the infraspinatus and the teres minor. These muscles are responsible for many of the motions of the shoulder. The large muscle that is more superficial than these muscles is the deltoid muscle. The shoulder joint proper is made up of the head of the humerus and the glenoid which is the socket and is actually a part of the scapula or wing bone. The glenoid is circumferentially lined by a thick fibrous ligament called the labrum. The clavicle (collar bone) joins the roof of the shoulder, the acromium (which is also part of the scapula), to form the acromioclavicular (ac) joint.
The rotator cuff muscles are relatively small and can be injured by an acute stress that exceeds their tolerance. Degeneration of the rotator cuff tendon also occurs from chronic use when the body’s rate of tissue damage exceeds the rate of repair. This is a normal part of the ‘maturing’ process. In the population at large about 25% of people age 40-60 years old have partial thickness rotator cuff tears. By age 60, 28% of the population has a full thickness tear (all the way through a portion of the tendon) and by age 80 over half the population has a full thickness tear. It is estimated that 72% of people with a full thickness tear have no symptoms and don’t know they have a rotator cuff tear. As we age, the thickness and quality of the tendon tissue deteriorate. The labrum also wears over time and a very large percentage of patients over 40 have some tearing of the labrum and most do not have any awareness of this phenomenon. There are secondary changes that occur in the shoulder concurrent with rotator cuff degeneration including bone spurs of the acromium and the ac joint. The obvious question is that if so many people have rotator cuff tears why do some have pain and dysfunction and others do not. This is not well established but there are many theories about this that have do to with the geometry of the tear, the basic anatomy of the individual and the stresses that are placed on the shoulder. It is also why, even with a full thickness tear, sometimes the right treatment is not surgical repair. Also, most labral tears do not have to be treated surgically although there are some that require it.
The initial evaluation involves a history, physical exam and usually specific x-ray views to assess the bone pattern and integrity of the shoulder. The treatment will often involve rest, heat, oral anti-inflammatory (non steroidal such as advil and alleve), cortisone injections in specific areas of the shoulder and eventually physical therapy. These treatments work gradually and require patience by the physician and the patient. Somewhere between 50-80% of patients even with full thickness tears can respond to non operative treatment. There are some patients who do not respond to these treatments and they require further evaluation.
The most commonly used test to evaluate the integrity of the rotator cuff is the MRI (magnetic resonance imaging). There is an assumption by the public that MRI testing is very exact and dependable. This is not always the case. MRIs like all tests are dependent on the quality of the MRI machine and the computer software that is used as well as the interpretive skills. In general larger magnet and non open MRI give superior images. Specific magnetic coils for certain body parts improve the imaging. Even given this, it is estimated that over half of partial thickness tears are not found on conventional MRI. Recent reports presented at the American Academy of Orthopaedic Surgeons Meetings indicate that MRI differentiates full from partial thickness tearing only fifty percent of the time which is no better than a flip of the coin. When needed, to improve accuracy, an MRI arthrogram (gadolinium is injected into the shoulder joint, not intravenous gadolinium) has significantly improved the accuracy of the test. The high false positive test rate with MRI without may have lead to many people having surgery for what is suspected to be a full thickness tear when they only had a partial thickness tear.
There are times when surgical intervention becomes the correct treatment. There are a number of different procedures based on the pathology. Generally, with partial thickness tears that have not responded to non-operative treatment the choice is arthroscopic surgery with debridement (shaving of the frayed tissue) of the rotator cuff often combined with removing bone spurs on the underside of the acromium. If there is significant arthritis in the ac joint that is symptomatic, a short section of the end of the clavicle may be removed at the same time. When a patient has a full thickness tear, the options are arthroscopic or mini-open rotator cuff repair. There is still debate about which procedure is more effective. The quality of the repair of the tendon with the mini open is felt to be stronger earlier because it is done through what are call interosseous tunnels. Arthroscopic repair is dependent on inserting anchors in the bone to which sutures are attached. It is a misconception that the rehabilitation is any longer or more difficult with one versus the other. In the long run the repairs seem to have equivalent results with success of repair and range of motion. It is however important to note that over 50% of rotator cuff repairs have some retearing of the tendon within one year of surgery, most without any symptoms. There is no correlation between the integrity of the repair and the resolution of patient symptoms. There are some rotator cuff tendons that can’t be repaired because the muscles have atrophied too much or the tendons have retracted or fibrosed and cannot physically be repaired.
This is meant to be a general overview and not an exhaustive discussion of rotator cuff pathology. I hope that it makes the issues clear and that I have corrected some misconceptions and given a candid view of what we know and what still needs to be worked on. I will be more than happy to discuss any of this information with you.
– Edward Bieber, M.D.
Related Content
- Can a Rotator Cuff Tear Heal Without Surgery?
- Can You Drive After a Rotator Cuff Repair?
- Complete vs. Partial Rotator Cuff Tears
- Rotator Cuff Disorders: The Facts
- The Difference Between Rotator Cuff Tears and Shoulder Tendonitis
- Types of Rotator Cuff Tears
- When Not to Have Rotator Cuff Surgery
- Shoulder Pain – Frozen Shoulder
- How to Avoid Shoulder Pain While Playing Golf
- Why Sleeping on Your Side Is Killing Your Shoulder
- Shoulder Pain – Cervical Spine
- The Ultimate Guide for Shoulder Recovery Surgery
- Does a Broken Shoulder Need Surgery?
- How Dr. Craig Miller Uses New Technology to Improve Shoulder Surgery
- Shoulder Arthritis and Shoulder Replacement
- How to Sleep After Shoulder Surgery
 ">
">
Get In Touch
Contact OrthoBethesda Today!
Whether you’ve received a referral from your primary care physician or would like to visit our premier team to discuss any orthopedic issues you may be experiencing, we invite you to contact us today. Patients in Bethesda, MD, Arlington, VA, and beyond can give us a call at (301) 530-1010.