Arthritis is a chronic condition that can cause life-altering pain for those who struggle with it. The Centers for Disease Control and Prevention (CDC) indicates that 54 million people — 23 percent of all adults in the U.S. — have arthritis. Around 24 million of those affected by arthritis are limited in the activities they can perform, and more than one-quarter of arthritis sufferers report that their joint pain is severe.
There are more than one hundred specific types of arthritis, each with their own range of symptoms, and it’s impossible to pinpoint everything that causes arthritis. Most types of arthritis can affect different parts of the body such as the hands, feet, knees or other joints. Understanding the most common forms of arthritis can help you better describe your condition to your doctor and make your treatment options clearer.
What Is Arthritis?
The word “arthritis” comes from the Greek “arthr-“, meaning “joint,” and “-itis”, meaning “inflammation.” It refers to scores of different diseases which usually impact areas in and around your joints. Muscles and tendons are frequently affected. Certain types of arthritis can also affect other body parts, such as how psoriatic arthritis is associated with psoriasis of the skin.
Arthritis is characterized by stiffness, pain and persistent fatigue. It doesn’t feel the same to every person, and a single person can experience significant variation in the severity of their symptoms from day to day. Some people may experience just a bit of pain in one or two joints, while another person’s whole body can be affected.
Most types of arthritis create symptoms at the joint. A person may experience swelling and tenderness along with warmth or redness in their joints. In some cases, joint pain occurs alongside weight loss and general weakness. Other symptoms are usually tied to the specific type of arthritis a person has.
Osteoarthritis
Of the two most frequently diagnosed types of arthritis, osteoarthritis (OA) is the most common. It generally affects middle-aged and elderly people, leading to the common misconception that it is simply “wear and tear” from a lifetime of using one’s joints. However, advances in OA research show that it affects ligaments, joint lining, cartilage and even bone.
Osteoarthritis involves the breakdown of the cartilage that acts as a cushion between the ends of your bones. It also deteriorates tendons and ligaments while causing inflammation of the joint’s lining. OA is one of the most common types of arthritis in the hands, hips and knees. Of the different types of arthritis in the back, osteoarthritis is the most common.
A person’s lifetime risk of developing one or more types of osteoarthritis differs based on the joint in question. The chance of OA in the knee is 46 percent and the risk of developing it in the hip is 25 percent. This arthritis type is one of the leading causes of disability in seniors. There is no way to cure osteoarthritis, and treatments are usually aimed at reducing pain and improving joint function.
Some of the ways you can manage the symptoms of OA include the following:
- Ensure your neck and back are supported for proper alignment while sleeping or sitting down.
- Make adjustments to the furniture for accessibility, like raising your toilet seat or chairs.
- Avoid making repeated bending motions of the joint when possible.
- If you are overweight, losing weight can reduce your pain and slow OA’s progression.
- Ask your doctor about adaptive devices to make daily activities easier.
Physical and occupational therapists can help you choose assistive devices and suggest the best exercises to manage the condition.
Rheumatoid Arthritis
This is one of the most debilitating types of arthritis as well as one of the most common autoimmune arthritis types. More than 1.3 million Americans have rheumatoid arthritis (RA), with about 75 percent being women. Somewhere between 1 and 3 percent of women get arthritis in their lifetimes. While RA can appear at any age, the disease most often starts between 30 and 50.
As an autoimmune disease, RA causes the immune system to attack the body — particularly the joints. It causes pain, stiffness and swelling in the joints, and decreases the joints’ range of motion. The most common types of rheumatoid arthritis strike in the small joints of the hands and feet. RA is one of the worst types of arthritis in finger joints. In some cases, RA can create a range of symptoms in organs including the skin and the eyes.
Stiffness is often markedly worse in the morning. It can last a couple of hours or all day. When possible, movement of the joints often helps. The long morning stiffness is uncommon in other types of arthritis, so it can be a strong indicator that you have RA. Other symptoms include:
- Lack of energy
- Low-grade fevers
- Lack of appetite
- Dry eyes and mouth
RA can also create firm lumps underneath the skin, known as rheumatoid nodules. They usually appear near affected joints.
There is no cure for RA. Treatment plans are designed with the goal of managing pain and increasing your ability to perform everyday tasks. People usually start with disease-modifying antirheumatic drugs (DMARDs). These drugs can relieve symptoms and slow down the disease’s progression.
In severe cases, doctors may prescribe medications categorized as biologic response modifiers. They block the signals in the immune system that cause inflammation and damage the joints and tissue. The downside to these medications is that they make it much easier and more dangerous to pick up something like a common cold.
Living with RA requires a careful balance of rest and physical activity. While stretching and low-impact aerobic exercises can help keep joints flexible, it’s important to scale back exercise when you experience a flare. The frustration that a chronic disease like RA can cause makes it a good idea to enlist the help of a mental health professional in addition to your medical team.
Psoriatic Arthritis

Psoriatic arthritis (PsA) is another autoimmune disease related to psoriasis. Psoriasis causes the immune system to attack the skin, resulting in scaly patches of red and white. About 15 percent of people with psoriasis will develop PsA. This arthritis can affect any joint, and the number of joints affected varies from person to person. The level of pain and stiffness in affected joints tends to fluctuate from day to day.
When present in the spine, one of the psoriatic arthritis types is called spondylitis. Psoriatic arthritis can also cause a condition called enthesitis, which creates tender spots at the points where tendons or ligaments connect to bones. It commonly causes pain in the elbows and feet.
Treatment of PsA differs based on how bad the pain and stiffness is. If you only have mild PsA in one or two joints, you may only need treatment during flare-ups. The first line of defense is usually a non-steroidal anti-inflammatory drug (NSAID) like ibuprofen or Aleve.
If the condition doesn’t improve, a doctor may prescribe a DMARD. There are also several biologic medications that can be administered by way of an infusion or an injection. Some of the available medications include:
- Humira
- Enbrel
- Simponi
- Remicade
- Cosentyx
- Stelara
Corticosteroid injections can help with excessive swelling.
Psoriatic arthritis has some broad implications for overall health. People with this condition are a little more likely to struggle with high blood pressure and cholesterol, as well as diabetes. A PsA treatment plan often takes these factors into account for a more comprehensive approach.
PsA usually develops in people between the ages of 30 and 50, but some children get it too. When they do, they are at risk of developing inflammation of the eye’s middle layer, called uveitis. Without treatment, uveitis can cause blindness or reduced vision.
Fibromyalgia
Fibromyalgia is a condition which causes widespread pain that can drastically lower a person’s quality of life. It manifests in pain and stiffness throughout the body and comes with other symptoms such as:
- Tiredness and fatigue
- Anxiety and depression
- Problems sleeping
- Problems thinking, remembering and concentrating
- Headaches and migraines
- Digestive problems or irritable bowel syndrome (IBS)
People suffering from fibromyalgia may also experience numbness or tingling in the extremities. This condition sometimes causes pain throughout the face or jaw. Disorders of the jaw are known as temporomandibular joint syndrome (TMJ).
Possible risk factors for fibromyalgia include:
- Obesity
- Repetitive stress injuries
- Illness
- Family history of the disease
- Traumatic events
You are more likely to get fibromyalgia as you get older and women are twice as likely to have the condition. Having lupus or RA is also a significant risk factor for fibromyalgia.
This condition has several associated issues that make it particularly difficult to live with. People with fibromyalgia are twice as likely to be hospitalized and often have co-occurring arthritis of another variety. Fibromyalgia is associated with higher rates of mental illness. Adults with the condition are more than three times more likely to have major depression than people without it, and fibromyalgia patients have higher death rates from suicide.
It is possible to treat fibromyalgia effectively with a combination of medical care and self-management strategies. Physicians may prescribe pain relievers or suggest over-the-counter options. In addition, they generally recommend:
- Aerobic exercise
- Exercise that strengthens muscles
- Patient education classes
- Stress management techniques
- Strategies for better sleep
In order to treat the depression that commonly accompanies fibromyalgia, doctors may recommend cognitive behavioral therapy (CBT). CBT is a form of talk therapy with the goal of changing negative thought patterns and behaviors.
Gout
Gout is one of the particularly painful arthritis types and has the ability to disable a person. This type of arthritis has been recorded for thousands of years, and has sometimes been called the “disease of kings.” This misleading name refers to the fact that gout has been incorrectly attributed to indulging in rich foods that only the wealthy could afford. In reality, anyone can get gout.
This arthritis is the result of uric acid building up in the body. The acid buildup causes crystals to form in the joints. In some cases, this happens because the body increases its production of uric acid. More commonly, it happens because the kidneys are not functioning at full capacity and cannot eliminate the uric acid well enough.
Here are some food and drugs that increase the risk of developing gout:
- Foods high in purines such as shellfish, red meat, organ meats and gravies
- Alcohol
- Fructose-rich foods and drinks like soda or candy
- Low-dose aspirin
- Diuretics
- Immunosuppressants used in organ transplants
Gout usually starts with intensely painful swelling in the joints, often causing the site to become red and warm to the touch. About 50 percent of first episodes happen in the big toe, and the rest of the foot is frequently affected. Gout is one of the more common types of arthritis in feet. However, gout can affect any joint.
Gout often flares up and then goes away. You can go to bed one night feeling normal, but wake up with extreme pain the next day. However, gout can become a chronic condition that affects you every day if not treated.
This arthritis is particularly difficult to diagnose, as different types of arthritis can mimic it. Testing for this disease is often done by looking for uric acid-based crystals. Doctors will often use extract some fluid from the affected joint with a needle, then examine the fluid with a microscope to find any crystals that may be present. Other forms of diagnosis involve examining patterns of joint involvement, blood tests and advanced imaging tests.
There is a variety of treatments available for gout. During active flare-ups, the medication colchicine can be highly effective. However, it has to be administered early in the attack to work, and the side effects are unpleasant. You may experience nausea, vomiting or diarrhea, among other side effects.
The NSAIDs indomethacin and naproxen are often the treatment of choice for gout attacks. The fastest symptom relief comes from short-acting NSAIDs in high doses. For people who can’t take NSAIDs, corticosteroids like prednisone are a good option. Depending on the number of joints affected, the medication can be injected right into the joint.
Gout pain can be reduced with cherry products. Eating a few cherries or drinking unsweetened cherry juice can help reduce the number of gout flare-ups, and drinking skim milk helps lower uric acid over time.
Lupus
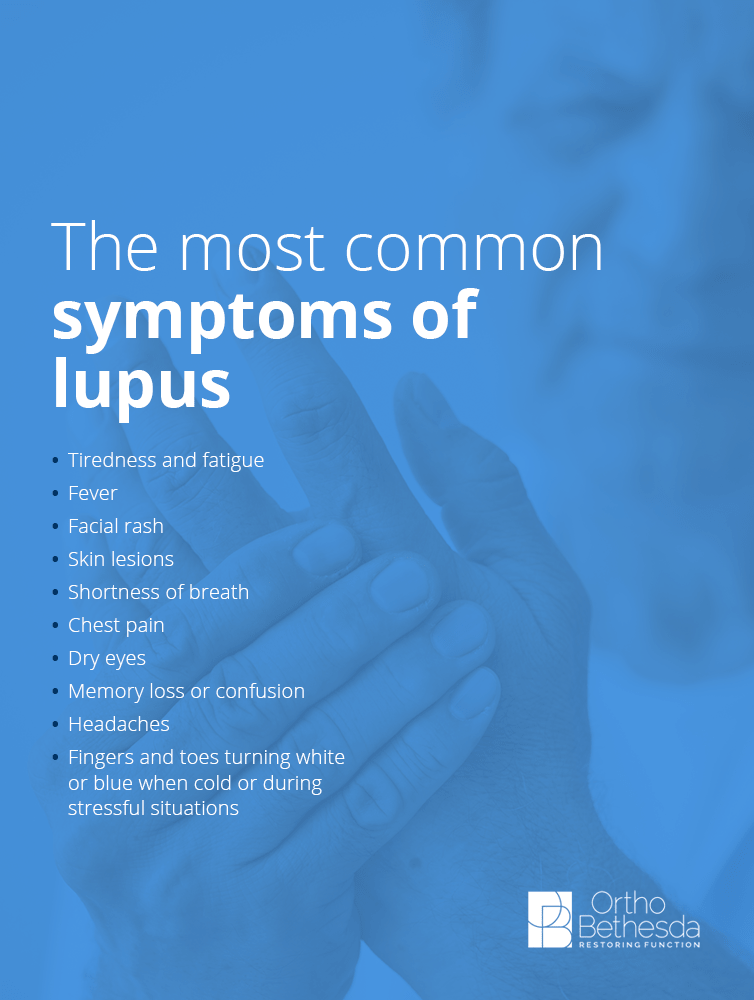
Lupus is another autoimmune disease that causes the immune system to turn against the body. It’s a systemic condition, which means it can damage any part of the body with the inflammation response. It most commonly affects the skin and joints, but can damage other organs like the kidneys, heart and lining of the lungs. The most common symptoms of lupus are:
- Tiredness and fatigue
- Fever
- Facial rash
- Skin lesions
- Shortness of breath
- Chest pain
- Dry eyes
- Memory loss or confusion
- Headaches
- Fingers and toes turning white or blue when cold or during stressful situations
For most people, lupus is active sometimes and mostly quiet the rest of the time. When the disease isn’t active, the patient’s state is referred to as a remission. Lupus flare-ups may be triggered by exposure to the sun and infections. Certain blood pressure medications, anti-seizure medications and antibiotics may also trigger lupus. Drug-induced lupus often gets better when the person stops taking the medication.
There is no cure for lupus. Treatment plans for this chronic disease are designed to suppress the immune system into a normal state of activity. People suffering from lupus have a few medication options:
- Hydroxychloroquine: Under the name brand Plaquenil, this antimalarial drug can treat arthritis induced by flare-ups as well as fatigue, rashes and mouth sores. It also helps prevent flare-ups.
- Corticosteroids: These are usually used when patients are dealing with serious symptoms like inflammation of the kidneys, lungs or heart.
- Immunosuppressants: These drugs help keep the immune system under control. Name brands include Imuran, Cellcept, Cytoxan and Rituxan.
- NSAIDs: For the pain caused by lupus flares, medications like ibuprofen and naproxen are good management tools.
- Biologics: There is one biologic approved by the Food and Drug Administration (FDA) for the treatment of lupus. Belimumab was approved for adults in 2011 and for children in 2019.
It’s very possible for people with lupus to live healthy and happy lives with appropriate treatment. Forming a support system and getting involved in your treatment by learning about the condition is a good first step. Seeing your rheumatologist regularly can help prevent serious issues or complications with the disease.
Staying active is essential for reducing joint pain and stiffness from lupus. Exercise helps your joints retain flexibility longer. Low-impact aerobics is a critical tool in reducing arthritis from lupus.
Tendinitis and Bursitis

These two conditions involve the inflammation and degradation of soft tissues near bones and muscles. Tendons are the fibrous cords that attach your muscles to your bones. Tendinitis inflames tendons, most often near the shoulders, elbows, wrists, heels and knees. It is often a result of “overdoing it” in sports, leading to nicknames like tennis elbow, pitcher’s shoulder or jumper’s knee.
The pain from tendinitis is often described as a “dull ache,” especially during movement. There is also tenderness and some swelling to contend with.
The bursa is a small sac filled with fluid that provides a cushion for the bones, tendons and muscles surrounding your joints. Bursitis is the term for when bursae experience inflammation. A joint affected by bursitis will feel stiff and ache. It may also look swollen or red, and hurt more as you move it or touch it.
The treatment for these common types of arthritis is usually rest, ice and NSAIDs. If the injured joint doesn’t receive rest, it will continue to show symptoms. Depending on the joint, resting it may be easy or difficult. If the issue is in your leg, hip or foot, you may need to limit walking for a while.
If tendinitis or bursitis persists in the face of standard treatment, physical therapy may be necessary. The physical therapist can give you a list of exercises that will help improve flexibility and retain function. If the problem continues to bother you, it may be time to visit a rheumatologist to see if another condition is developing.
Orthopedic Care for Arthritis
Most types of arthritis can be managed with help from medications, exercise and tips from a physician or rheumatologist. But in some cases, surgical intervention may be required. For example, an older person with severe osteoarthritis of the hip may not be able to live a full and functional life without having the hip replaced.
The process of orthopedic treatment can feel frightening, which is why it’s crucial to find a treatment center that puts your needs first. OrthoBethesda takes a uniquely conservative approach to treatment to ensure we don’t perform any unnecessary invasive treatments.
When you come in for your first appointment, we thoroughly evaluate your condition and formulate a plan that is specific to your needs. Oftentimes, this will include taking x-rays to get a clearer picture of whether surgery is necessary. If it’s not imperative, we provide other options such as physical therapy or corticosteroid injections. Our goal is to do everything in our power to improve your arthritis symptoms through non-invasive means whenever possible.
If the condition doesn’t respond to our treatment, we will walk you through a surgical solution. We know how important it is to answer your questions and paint a clear picture of how the solution can improve your condition.
Living with any of the different arthritis types is painful, and the best orthopedic care focuses on relieving that pain. If you’re ready to learn more about OrthoBethesda, our team of orthopedic experts or our services, we invite you to contact us online or give us a call at (301) 530-1010. You can even set up an appointment online for greater convenience.
Related Content
- Arthritis vs. Arthrosis
- Types of Bursitis
- Consequences of Delaying Medical and Surgical Care
- Winter Injury Prevention Guide
- Inpatient Surgery vs. Outpatient Surgery
- Why Your Joints Are Cracking
- What Does an Orthopedic Doctor Do?
- How to Prevent Osteoporosis
- Types of Common Outpatient Surgeries
- What to Wear and What Not to Wear During Surgery
