Your spine provides your body with proper support and structure, connecting various aspects of the musculoskeletal system. The spine plays an essential role in every activity we perform, including standing, sitting, twisting and walking. The spine is made up of the backbones, which are commonly known as the vertebrae. Between each vertebra is an intervertebral disc that cushions these bones and absorbs shock from various movements. When a disc is injured, it can result in pain, discomfort and even limited mobility.
What Is a Herniated Disc?
A herniated disc, often referred to as spinal disc herniation or a prolapsed disc, is a condition that affects your spinal discs or the rubbery cushions which separate the individual vertebrae of the back. A healthy spinal disc has a nucleus, which is a soft, jellylike center encased in a rubbery exterior known as the annulus. When the nucleus pushes through and tears the annulus, the resulting condition is known as a herniated disc.
A healthy spinal disc helps absorb shock from various activities, like walking, hopping, twisting or other daily actions. When a disc becomes herniated, it cannot function properly, leading to two vertebrae coming into contact or painfully grinding against one another. While pain and discomfort are common symptoms of a herniated disc, some patients may also experience a spinal nerve being pinched or compressed, leading to potential numbness or pain along the affected nerve.
How Painful Is a Herniated Disc?
One of the most common symptoms of a herniated disc is pain or discomfort. Over time, an untreated herniated disc can lead to sensitive nerves, severe pain and even nerve compression or damage. In some of the most severe instances of a herniated disc, the disc may slip and block nerve impulses in your lower back and legs. How long a herniated disc takes to heal depends on the severity of your symptoms and how soon you seek proper treatment.
One of the most important aspects to consider is what activities you should avoid with a herniated disc. Certain movements can aggravate herniated disc symptoms and worsen the overall health of the affected vertebrae and spinal discs. A spinal specialist can help determine the severity of your symptoms and recommend avoiding certain activities to promote spinal healing. In many cases, you should limit or eliminate heavy lifting or intense physical activity until the herniated disc heals.
What Causes a Herniated Disc?
In some cases, a herniated disc may not initially lead to discomfort, pain or other noticeable symptoms, making it essential that you understand how you get a herniated disc. Without noticeable symptoms, some patients may wonder what a herniated disc feels like. Spinal discs have very little innervation, meaning many patients do not feel pain until the herniated disc affects nearby structures, such as nerve roots, muscles or joints.
Some of the most common risk factors and causes of a herniated disc include:
- Age: One of the leading causes of herniated discs is aging. Over time, the discs experience wear and tear related to old age. As a result, the spinal discs become less flexible and are more prone to rupture or herniate from minor movements. Herniated discs are most common in patients in their third to fifth decade of life.
- Excess weight: Excess weight can be a risk factor that increases the potential for a prolapsed disc. With excess weight, your spinal column and discs are under greater pressure and stress, leading to a higher risk of injury, spinal compression and other issues associated with a herniated disc.
- Disc dehydration: At birth, your spinal discs mainly comprise water. With age, these spinal discs begin to thin and lose this essential water. Dehydrated discs are less effective at absorbing shock and cushioning the vertebrae. Thinner spinal discs can increase the risk of spinal complications and herniation.
- Genetics: Genetics play a direct role in determining if you are more prone to certain spinal conditions, such as herniated discs. There is a hereditary tendency for disc degeneration that is directly associated with an increased risk for prolapse. A family history of disc degeneration or herniated discs may point to a potential future herniation.
- Occupational hazards: Certain jobs may increase your risk of experiencing a herniated disc. Active, physically demanding jobs often carry a larger risk of spinal problems or certain back conditions. If you regularly work with heavy materials, you may be more likely to develop a prolapsed disc.
- Repetitive movements: Repetitive movements can add stress and strain to your back over time. Repetitive movements that may lead to a herniated disc include continuously bending, pulling, lifting, twisting or pushing. Repeating these movements over a long period of time can cause wear and tear on the discs and increase the possibility of herniation.
- Smoking: A history of smoking and tobacco use can increase your risk of developing a herniated disc. When you smoke, the oxygen supply to your spinal discs decreases, increasing the likelihood that the disc will degenerate more quickly and may experience other complications.
- Traumatic injury: In some cases, a traumatic injury or accident can lead to a herniated spinal disc. If an accident involves stress, tension or injury to the back, a spinal disc may become dislodged or herniated.

9 Signs You Have a Herniated Disc
You might wonder how to tell if you have a herniated disc. While a medical diagnosis is always necessary, knowing the most common herniated disc symptoms can help determine if you should see a spinal specialist. It’s also useful to understand when a herniated disc produces symptoms, which can help you determine if recent back pain, neck pain or other symptoms may be caused by a potential disc injury.
While herniated disc symptoms vary from patient to patient, some of the most common signs of a herniated disc include:
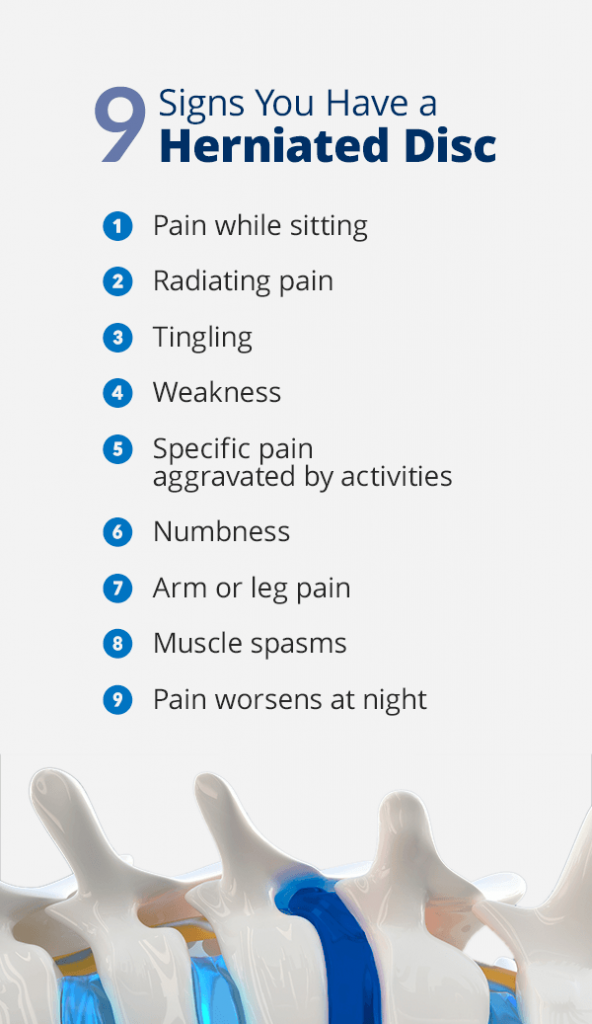
1. Pain While Sitting
In many cases, a herniated disc may cause worsening pain when physically active during the day. Unfortunately, a common symptom of a herniated disc is pain, even when sitting or while at rest. Sitting places a large amount of stress and strain on the lower back and spine. With increased pressure, the herniated disc may become more noticeable and pronounced.
Many people with a herniated or prolapsed disc may notice that sitting for long periods of time can worsen painful symptoms. In general, avoid prolonged sitting to prevent pressure and strain on herniated discs. Proper spine alignment can help ease spinal pressure and reduce the overall level of discomfort you may feel when sitting.
2. Radiating Pain
When a spinal disc herniates, it often occurs near the sensitive and delicate spinal nerve roots. There are two forms of spinal irritation herniated discs may cause, including direct compression and chemical irritation. With direct compression, the inner contents of a leaking spinal disc may apply pressure to the spinal nerve root as it exits the spinal canal.
On the other hand, chemical irritation may also occur due to a herniated spinal disc. The internal contents of a spinal disc comprise acidic chemical irritants that may inflame or irritate the nerve root. If the nerve root is compressed or irritated, then the functioning of the nerve root is altered, causing pain to radiate through the body, especially through the thighs, legs and even the feet. This pain may be referred to as sciatica.
3. Tingling
Herniated discs in the lumbar spine often cause a tingling sensation to develop, affecting one or both legs. If a herniated disc is located higher in the spine, it may lead to a sensation of tingling up the neck or down the arms to the hands. Tingling paired with discomfort and pain from a herniated disc can make daily tasks difficult. Tingling is often directly associated with a sensation of numbness or general weakness.
4. Weakness
Herniated discs can directly impact the health and functioning of the nearby nerves and nerve roots. A general sensation of weakness is a common symptom of a herniated disc that causes compression or strain on nearby nerves. The location of the herniated disc plays a large role in potential symptoms. Herniated discs located nearby spinal nerves can result in weakness or numbness.
In many cases, a feeling of weakness develops in one or both of the legs and potentially in the arms. While weakness and numbness can be uncomfortable in general, they often complicate a person’s day. If someone feels a sensation of weakness in their legs or arms, they may have difficulty performing certain actions or activities.
5. Specific Pain Aggravated by Activities
Pain and discomfort from a herniated disc may occur or worsen when you perform specific activities that place additional strain on the lower back. Activities that aggravate herniated discs include bending down or forward, twisting the body and pushing or pulling objects.
Even daily activities or actions, such as sneezing or coughing, can aggravate herniated disc symptoms. Those with a herniated disc should also avoid lifting heavy objects or performing repetitive actions directly impacting the spinal column and discs. Herniated disc pain and discomfort can be quick and severe when performing an action that causes pressure on the herniated disc.
6. Numbness
Herniated discs can cause a feeling of radiating numbness in various parts of the body. The location of the numbness depends on the site of the herniated disc and the affected nerves. In many cases, people notice numbness developing in the arms or legs that may even extend to the feet or hands.
Numbness is an uncomfortable and distracting feeling that often makes focusing on important tasks difficult. A sense of numbness can cause people to stumble or have difficulty walking. Many people may also experience difficulty performing various daily tasks, such as driving if they notice numbness in their hands or fingers.
7. Arm or Leg Pain
While lower back pain is a common side effect of a herniated disc, many people may also notice discomfort or pain in the arms and legs. Herniated discs in the lower back may cause pain in the buttocks, thighs, calves and even the feet. Herniated discs of the upper back and neck may cause pain in the shoulders, upper arms, lower arms and hands.
Some people may experience arm or leg pain regularly due to their herniated discs. Others may only experience arm or leg pain when they perform an action that causes strain on the herniated disc, such as sneezing, coughing or moving into a position that causes pressure on the herniated disc. While individual symptoms may vary, many people describe arm or leg pain as burning or sharp.
8. Muscle Spasms
Muscle spasms are a possible side effect and symptom of a herniated spinal disc. When a disc herniates or bulges, it can compress nearby spinal nerves and nerve roots. When a spinal nerve root is compressed, irritation and inflammation often occur. In some cases, your body tries to immobilize the affected area and reduce pain by contracting and tightening surrounding muscles, leading to uncomfortable and painful muscle spasms.
9. Pain Worsens at Night
Many patients may notice that they experience higher levels of pain at night. Like sitting, lying down can cause additional stress and compression on a herniated disc. Your sleeping posture and position are important aspects to consider when trying to sleep with a herniated disc. Stomach sleepers may be more prone to herniated disc pain, as this position puts strain on the cervical spine.
Certain sleeping positions have also been known to increase the arch of the lower back or the neck, leading to worsening pain if a herniated disc is located in these parts of the spine. Proper support and healthy sleep posture are important elements of getting a good night’s rest with a herniated disc. While the ideal sleeping position varies from patient to patient and depends on the location of the herniated disc, many people experience more comfort when attempting to sleep on their back.
When to See a Doctor for Your Symptoms
Understanding what a herniated disc looks like and the symptoms it causes can help you determine if you should seek medical attention. A spinal specialist can provide numerous benefits. A medical professional can explain how long it takes for a herniated disc to heal, and they can recommend potential treatments or lifestyle changes to improve your symptoms.
If you are experiencing long-term back pain, it is always a good idea to seek medical attention. Patients should see a doctor if symptoms inhibit their ability to perform certain actions or cause a large negative impact on their daily lives.
If you experience severe pain, pain that radiates or travels down the legs and arms or if you experience prolonged weakness, tingling or numbness, you should see a doctor to evaluate these symptoms. Fortunately, a spinal specialist can provide treatment suggestions to help alleviate the severity of these symptoms and improve pain caused by a herniated disc. If a person does not seek medical attention for a herniated disc, they run the risk of experiencing potential complications, including:
- Chronic pain: As pain is one of the most common symptoms of a herniated disc, those who do not seek medical attention are likely to experience chronic or long-term pain. Chronic back pain can be difficult and inhibit a person’s ability to perform daily activities while negatively impacting a person’s overall quality of life. Without treating a herniated disc, this pain is likely to continue and even worsen over time.
- Nerve damage: If a herniated disc compresses or adds pressure to nerves or nerve roots, there is potential for long-term nerve damage. In many cases, the longer nerve compression continues, the more severe symptoms become over time. Without proper treatment, some patients may experience permanent nerve damage.
- Saddlebag numbness: Saddlebag numbness, also known as saddlebag anesthesia, is a condition that describes numbness in the pelvic area that would come into contact with a saddle if you were to ride a horse. With saddlebag numbness, people may begin to lose feeling down the back of the legs, the inner thighs and the buttocks.
- Bladder and bowel incontinence: An untreated herniated disc can cause nerve damage and compression, directly impacting the bladder and bowels. In severe cases of a herniated disc without treatment, a person may lose the ability to control their bladder and bowels.
- Partial paralysis: Over time, pain and discomfort often worsen as a herniated disc remains untreated. In severe cases, a herniated disc can result in partial paralysis, largely impacting a person’s daily life.
How a Doctor Can Determine a Herniated Disc Diagnosis
A proper medical diagnosis is an important aspect of treating a herniated disc. Fortunately, a herniated disc can heal on its own in some cases. The most effective way to properly determine if you have a herniated disc is to seek professional medical attention. In many cases, a doctor can help determine if you are experiencing a herniated disc. There are numerous physical and medical tests available to help determine the source of back pain.
Some things a doctor may consider when diagnosing a herniated disc include:
- Leg strength: Stretch tests can help determine leg strength and provide useful information on diagnosing a herniated disc. Your physician may ask you to perform straight leg raises. If pain occurs when the leg is raised at certain angles, it can signify a herniated lumbar disc.
- Walking mannerisms: Another beneficial test is to monitor a patient’s way of walking and their gait mannerism. Observing how a person walks can help a physician determine if a patient may be walking slowly or favoring one leg due to pain, discomfort or a limited range of motion. An abnormal gait may be a simple sign of a herniated disc or spinal condition.
- Touch sensitivity: Touch sensitivity plays an important role in determining if you may be experiencing symptoms of a herniated disc. Your doctor will evaluate your overall touch sensitivity and decide whether you can feel various light vibrations or touches. A loss of sensation or numbness may indicate symptoms of a herniated disc or nerve compression.
- Medical imaging: In some cases, a doctor may want to rule out other complications or sources of pain. Further testing can help pinpoint specific pain areas or aggravated nerves. In some cases, your physician may suggest a medical imaging test, including an x-ray, CT scan, MRI scan or myelogram.
How to Heal a Herniated Disc
After being diagnosed, your next question is likely how to cure a herniated disc. There are numerous ways to treat a herniated disc and alleviate painful and uncomfortable symptoms. Learning what to do for a herniated disc can help ease painful symptoms, improve a proper range of motion and enhance your overall quality of life. In most cases, a doctor will recommend non-invasive and non-surgical treatments. Some of the most effective treatments to fix a herniated disc include:
- Medication: One of the most common ways to fix a herniated disc in the lower back is nonsteroidal anti-inflammatory medications, known as NSAIDs. Over-the-counter and prescription medication can improve painful symptoms associated with a herniated disc.
- Lifestyle changes: Many patients may wonder what to do about a herniated disc and assume they will only find relief from surgery. Fortunately, there are numerous lifestyle changes you can make to improve symptoms of a herniated disc. Physical exercise and a healthy diet can improve various symptoms of a prolapsed disc. Additionally, a heating pad can also provide soothing relief to a herniated disc.
- Physical therapy: Physical therapy can be a great way to strengthen weakened muscles and promote a healthier back. Certain movements and exercises can strengthen abdominal muscles and ease lower back pain.
- Spinal surgery: While non-surgical and non-invasive treatments effectively manage herniated disc treatments, some patients with more severe symptoms may require surgery. Spinal surgery may be needed if a disc fragment lodges itself in the spinal canal and compresses a nerve.
- Prevention: Learning how to prevent a herniated disc can help you maintain a healthy spine and avoid future injuries. Try to be mindful of proper posture and techniques for safely lifting heavy items.

Premium Spinal Treatment and Surgery
At OrthoBethesda, we are committed to providing innovative spinal treatments for various orthopedic conditions to improve our patients’ overall quality of life. Our doctors and surgeons, as well as our physician assistants, are highly trained professionals committed to providing innovative orthopedic care. All of our physicians are fellowship-trained in their unique specialties and well-respected in their fields.
To learn more about our orthopedic services, schedule an appointment or contact us online today.

Related Content
- How to Prevent Back Pain When Working From Home
- How to Reduce Low Back Pain
- How to Sleep After Back Surgery
- 10 Steps to Achieving Better Posture
- How to Sleep With a Herniated Disc
- Spinal Fusion Surgery – Commonly Asked Questions
- Spine Surgery: When It Works and When It Doesn’t
- Dr. Eric Feuchtbaum Makes Advancements in Minimally Invasive Spine Surgery With Mazor Robotics
- What Is Kyphosis?
- What Causes Sciatica Nerve Pain?
- Everything to Know About Scoliosis
